Like all tissues in our body, our heart muscles need oxygen and nutrients to function correctly. These nutrients and oxygen are delivered to the heart by a group of arteries covering our heart, known as Coronary arteries.
Coronary heart disease (CHD) is also called ischemic heart disease (IHD) or coronary artery disease (CAD). In CHD, heart muscles are deprived of oxygen due to the blockage of coronary arteries, leading to the death of heart tissues.
Oxygen deprivation is usually caused due to blockage of arteries by atherosclerosis, in which narrowing of coronary arteries occurs. The coronary artery’s cross-sectional size dramatically influences oxygen demand to myocardial muscles (heart muscles are called myocardium).
Any reduction in size due to plaque reduces the coronary artery’s cross-sectional dimension, resulting in reduced blood flow and reduced oxygen supply leading to oxygen deprivation.
Plaque depositing also sometimes diminishes the elastic ability of arteries to expand in response to increased myocardial oxygen supply.
Oxygen deprivation to myocardial tissues also occurs due to increased oxygen demand and less oxygen supply by blood; it may be due to ventricular hypertrophy due to hypertension or increased thyroid hormone. In both cases, myocardial tissue increases, resulting in increased oxygen demand.
- How are plaques formed?
- Factors Increasing Risk of Coronary Heart Disease:
- Complications due to Coronary Heart Disease:
- Symptoms of Coronary Heart Disease:
- Diagnosis of Coronary Heart Disease:
- How can coronary heart disease risk be reduced?
- Medicines Used in the treatment of Coronary Heart Disease:
- Ending Note:
How are plaques formed?
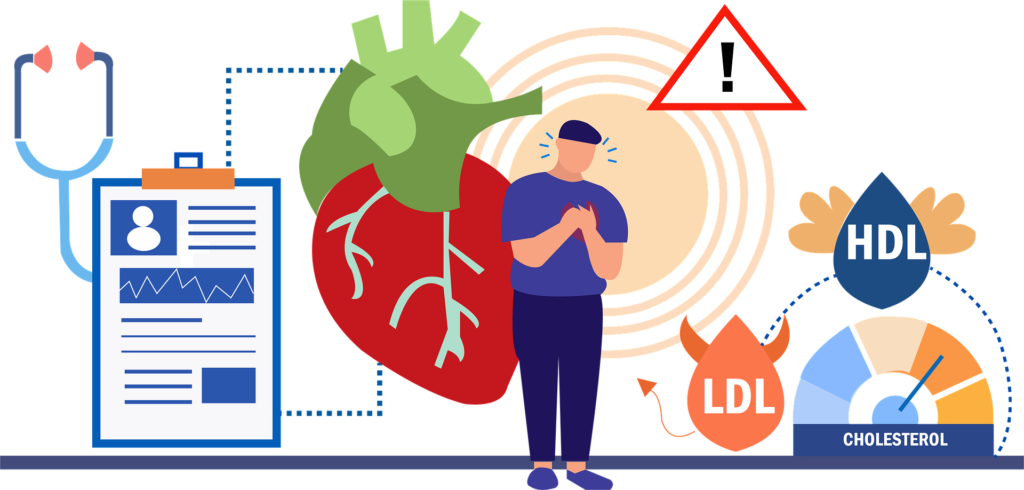
The Fatty Streaks of cholesterol can be found in individuals, even from a young age. Usually, plaques are formed due to increased blood cholesterol levels, resulting in oxygen deprivation.
This high cholesterol starts depositing the arteries causing their narrowing and thickening.
The formation of plaques doesn’t happen in days or weeks. It takes a long time in developing plaques, usually years or decades (beginning even in childhood or adolescence).
The plaque gradually builds up in coronary arteries getting bigger and bigger with time. This process of building up plaques in arteries is called atherosclerosis.
It is only felt when it starts obstructing the blood supply. Our heart needs a constant supply of oxygen for it to work; this plaque formation reduces the blood passing through coronary arteries,
Factors Increasing Risk of Coronary Heart Disease:
Several factors increase the risk of coronary heart disease; there are modifiable factors which we can intervene and reduce the risk associated. These modifiable factors are as follows,
- Cigarette smoking
- Raised serum cholesterol
- Hypertension
- Diabetes
- Abdominal obesity
- Increased personal stress
Other than modifiable factors, the occurrence of CHD also involves non-modifiable factors. These are the factors that we cannot control and are related to age, gender and family history as explained below,
Gender:
A study shows that more males are diagnosed with CHD than females of the same age group. The difference may be due to differences in male and female genetic makeup as both male and female body responds differently to certain diseases, environmental factors and emotional problems.
Males are more affected by obesity, hypertension, diabetes, stress, anger, depression, financial situations and anxiety related to it; these factors directly relate to the development of CHD.
Hormones:
Estrogen protects females from the harmful effects of fat deposition, reducing with increasing age. Females above 55 are more susceptible to developing CHD than men of the same age because of the absence of sex hormones in females after menopause.
Females undergoing hormonal replacement therapy after menopause suffer less from CHD as they take these hormones from an outside source.
Age:
Age is another non-modifiable risk factor, as it takes time for plaque build-up in arteries. As age advances, more cholesterol deposits in the body and coronary arteries with time.
Family History:
Family history plays a vital role in the development of CHD. If you have any first-degree relative who has CHD, then there are high chances that you will also have this problem.
The illness can be avoided by identifying families with a positive history of CHD, particularly in persons with parents or siblings with artery disease or who died due to a family history of CHD at a young age.
Complications due to Coronary Heart Disease:
If it is not controlled, CHD leads to many complications:
- Stable Angina
- Acute Coronary Syndrome
- Acute Myocardial Infarction
- Unstable Angina
- ST-elevation myocardial infarction
Symptoms of Coronary Heart Disease:
Patients should be asked about
- Chest pain and chest congestion during physical activity
- Radiation of the chest pain into the jaw, neck, left arm, or the back during physical activity
- Dyspnea on activity
- Syncope
- Palpitations
- Tachypnea
- Lower extremity oedema
- Orthopnea
- Reduced exercise capacity
Diagnosis of Coronary Heart Disease:
These examinations are performed based on the circumstances in which patients appear. To mention a few, the primary techniques for evaluating coronary artery disease include
EKG:
EKG is performed by attaching ten electrodes, often called leads, on the specific points of the chest according to the heart position in the body. The results are obtained, and the heart conduction system can be analyzed. It is a non-invasive procedure.
EKG or electrocardiogram is a helpful test used to test heart rate, rhythm, and axis of the heart. It provides information and helps in diagnosis of,
- Arrhythmias
- ST-segment changes and T wave changes of ECG
- Bundle branch block
- Ventricular hypertrophy
Echo:
Echo or Echocardiography is an ultrasound of the heart. It is expensive as compared to EKG. It provides information like,
- Artery stenosis
- Heart chamber sizes
- Heart activity evaluation
- Valvular regurgitation
This test is dependent on the user’s skill and can be used for various purposes in clinical settings. It is a non-invasive procedure.
Stress test:
Our body is exposed to artificial stress like running on the treadmill in a stress test. It is a non-invasive procedure and is commonly used to diagnose angina.
It is one of the most important diagnostic tests done to evaluate CHD.
The heart functions are then evaluated with the help of an EKG. The EKG readings are monitored; if there are abnormal readings and changes in the ST segment, the test is aborted, and at that point, CHD is diagnosed.
If there are no changes by the end of the test, the EKG readings are compared and recorded before the test, during, and after. The CHD is diagnosed if there are differences in the EKG found. Following symptoms are monitored for diagnosis of CHD;
- Hypotension or Hypertension
- Arrhythmias
- Abnormal ST-segment changes (Elevation or depression of ECG)
Apart from the physical stress tests, pharmacologic stress tests are also done.
Cardiac Catheterization:
This technique is performed in a cardiac catheterization lab, requires experience, and is performed under mild sedation. It is considered a Gold Standard for confirmation of CHD. It is an invasive procedure and is not bearable for every patient.
Other than EKG, Echo, Stress test and Cardiac catheterization following test also proves helpful in confirming the diagnosis of CHD;
Chest X-Ray:
It is a low-cost and simple tool for determining the severity of the cardiac disease. It provides information related to different organs of the body. The heart size position can be evaluated.
Blood tests:
Elevation of the cardiac enzyme (troponin) is monitored, disturbing and elevated in CHD. Apart from cardiac enzymes, LFTs, CRP, ESR, RFTs also helpful in confirming the presence of CHD.
How can coronary heart disease risk be reduced?
As coronary heart disease develops gradually with time, the risk can be reduced by
- Regular consumption of fresh fruit and vegetables
- Regular exercise
- Stopping alcohol consumption
Modification of factors that increase the risk of CHD: like
- Reducing cholesterol
- Controlling high blood pressure
- Reducing weight etc
Medicines Used in the treatment of Coronary Heart Disease:
Here is a list of drugs commonly used in the treatment of Coronary Heart Disease.
- NITRATES & NITRITES (Nitroglycerin, Isosorbide dinitrate, Nicorandil)
- CALCIUM CHANNEL-BLOCKING DRUGS (Amlodipine, Nicardipine, Diltiazem, Verapamil)
- BETA-BLOCKING DRUGS (Propranolol, Atenolol, Metoprolol)
- STATINS
- ACE INHIBITORS
- MISCELLANEOUS (Ranolazine, Ivabradine)
The details of these medicines, their mechanism of action, their benefits, their adverse effects, famous commercially available brands, their pharmacological class etc., are discussed in detail on their respective pages. Click on the medicine name to open the page you want to study.
Ending Note:
A mix of modifiable and non-modifiable conditions contribute to coronary artery disease. Controlling diabetes, hypertension, and cholesterol levels and quitting smoking, losing weight, and exercising can significantly impact. Primary care physicians should focus on modifiable risk factor management on each routine appointment.
References:
- Shahjehan RD, Bhutta BS. Coronary Artery Disease. [Updated 2022 Feb 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564304/
- Tabei, S. M., Senemar, S., Saffari, B., Ahmadi, Z., & Haqparast, S. (2014). Non-modifiable Factors of Coronary Artery Stenosis in Late Onset Patients with Coronary Artery Disease in Southern Iranian Population. Journal of cardiovascular and thoracic research, 6(1), 51–55. https://doi.org/10.5681/jcvtr.2014.010