Early diagnosis and treatment of heart failure is important so condition doesn’t worsen. Signs of heart failure such as shortness of breath, fatigue, or swelling can appear early in the disease process.
Sometimes, people have no symptoms. They may have a physical exam and tests that show whether the heart functions normally.
Diagnosis of heart failure is based on medical history, physical examination, and various tests. During the physical examination, your doctor will detect low blood pressure, an elevated jugular venous pressure (the jugular vein is the vein in the neck), abnormal heart rhythms and pulmonary congestion suggested by a chest X-ray.
The doctor can also listen to your heart and lungs with a stethoscope and detect the impaired heart sounds and abnormal breath sounds typical for heart failure.
Various techniques can diagnose heart failure, and the most common method involves listening to the heart and lungs via a stethoscope during a physical exam.
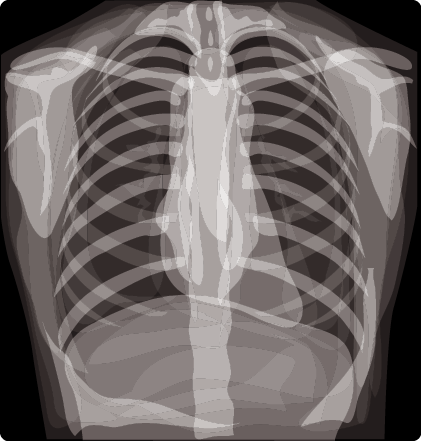
Chest X-Ray in the diagnosis and treatment of heart failure:
Chest X-ray, EKG, and echocardiogram are used to diagnose heart failure. A chest x-ray is a most frequently used test to diagnose heart failure.
The chest x-ray can help determine the size and shape of your heart and the condition of your lungs. These findings indicate whether the cause of heart failure is abnormal function or blockage of blood flow in the heart.
Echocardiogram:
Echocardiography employs ultrasound waves to create still and video pictures of the heart’s chambers, valves, and surrounding tissues. The most often used test to diagnose and measure the severity of CHF is echocardiography.
This test can estimate the pumping capabilities of your heart muscle, which allows your doctor to plan further treatment.
Echocardiography can also demonstrate how effectively your heart pumps blood. This test uses high-pitched sounds, or ultrasound, to take pictures of your heart. Your doctor will know if you have CHF based on these pictures.
Blood Tests:
There is an increase in the size of the heart in systolic heart failure, which causes an increase in the stretch of muscles. This increase in muscle stretches triggers the release of B-type natriuretic peptides (BNP) in the blood. More the presence of BNP in blood more severity of heart failure. It is measured in Pico grams per millilitre (pg/ml)
BNP levels in the blood can be predicted as follows,
- Less than 100 pg/ml – No Heart failure
- 100 – 300 pg/ml – Heart failure
- 300 – 900 pg/ml – Mild Heart failure
- Greater than 900 pg/ml – Severe Heart failure
Stress Test:
The stress test is performed for the complete diagnosis of cardiovascular diseases. It is a condition in which the patient is physically tested on a running machine, or in case of less mobility; they can be tested on a bicycle or have the leg movements with standing still.
Heart activity is monitored before and after this test. Diagnosis is based on heart performance under various conditions.
The exercise stress test or stress test is a diagnostic tool that can provide information about the function of your heart under physical exertion.
This can help detect abnormalities with heart function, including coronary artery disease or cardiac arrhythmias (abnormal heart rhythms) such as atrial fibrillation.
It is done for the diagnosis of heart failure, chest pains etc. This test is usually done in a hospital or clinic, and a provision for emergency treatment is available.
Treatment of Heart Failure:
The main objectives of therapy in heart failure are to keep the body supplied with oxygen, reduce symptoms progression and improve quality of life. It is essential to control risk factors that can cause heart failure, such as hypertension (high blood pressure) and coronary artery disease.
This can prevent heart failure or at least delay its progression. If heart failure occurs, it is essential to treat and adjust cardiac medications to address underlying causes, minimize symptoms and prolong life.
Treatment of heart failure consists of early-stage treatment and late-stage treatment.
Early Stage:
Early treatment is a symptom-free state, where risk factors for heart failure are modified to prevent the disease.
In the early stages, many factors can contribute to the pathogenesis of the cardiovascular disease. Certain factors such as hypertension and diabetes are potentially reversible.
Target risk factors which are treated:
- Hypertension
- Coronary heart disease
- Diabetes
Medications in Early Stages:
- ACE inhibitors
- Vasodilators
- B-Blockers
The treatment at an early stage may not include drugs, but your doctor would advise you to exercise and follow a healthy diet. These two elements are critical in reducing the development of risk factors such as hypertension, CAD, obesity, and diabetes, contributing to heart failure.
Late Stage:
In the late-stage treatment of heart failure, the underlying diseases can no longer be cured, but doctors can help you live comfortably with your condition. Your symptoms are best controlled by medicine, diet, and lifestyle changes in this stage.
Medications in Late Stages:
- Diuretics
- Calcium Channel Blockers
- Digoxin
- ACE inhibitors
- B- Blockers
Devices:
Devices used in managing our heart failure are ventricular assist devices, cardiac resynchronization therapy, Transcutaneous pacing, Implantable cardioverter-defibrillator, Cardiac pacemaker.
Ventricular Assist Devices:
As a supplement to more conservative heart failure treatments, patients may get a ventricular assist device (VAD), also called mechanical circulatory support (MCS) system or a bi-ventricular assist device (BVAD).
When your heart is weakened by damage, it cannot always pump enough blood to meet the body’s needs. A VAD temporarily helps a failing heart pump blood. It provides some of the pumping ability that your damaged heart can no longer provide.
The two major classes of ventricular assist devices are:
- Left Ventricular Assist Devices (LVADs)
- Right Ventricular Assist Devices (RVADs)
- VADs for both ventricles (BiVADs)
Even though these devices may help the quality of life and quantity of life, they may have complex complications to manage.
Cardiac Resynchronization Therapy:
A Cardiac Resynchronization Therapy (CRT) device is designed to help your heart pump more efficiently by sending electrical signals to both ventricles of the heart to coordinate their pumping actions.
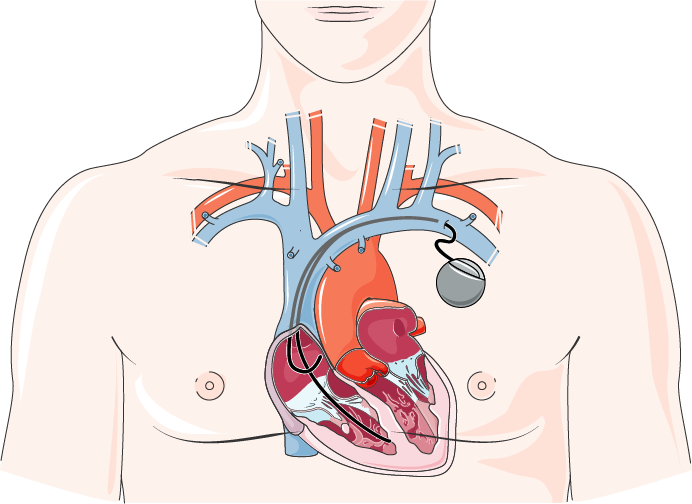
These carefully timed signals allow your heart to beat stronger and more efficiently with each contraction. CRT devices will also monitor your heart’s rhythm, and if a fast rhythm is detected, deliver a low-level shock to return the heart to its normal rhythm.
Devices includes
- Pacemakers
- Cardiac Defibrillator
A pacemaker and defibrillator are devices that send electrical signals to the heart through wires called leads. Pacemakers and defibrillators are devices that send electrical signals to the heart and help maintain a normal heart rhythm or treat an abnormal heart rhythm.
These devices help the heartbeat usually or treat an abnormal heart rhythm and are implanted beneath the skin in your upper chest by a surgeon. Sometimes, both a pacemaker and a defibrillator are needed to manage an arrhythmia or symptoms of heart failure.
Surgical Treatment of Heart Failure:
Surgical treatment of heart failure is evolving rapidly. It includes mechanical circulatory support devices, surgical stents, coronary artery bypass grafts, ventricular correction surgeries (including resynchronization devices), and complete heart transplants.