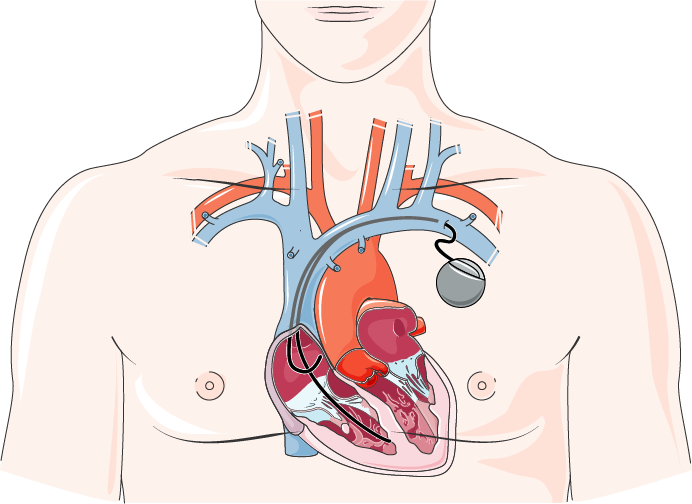
Throughout our lives, our heart functions as a pump. It distributes oxygenated blood from the lungs throughout our body, receives deoxygenated blood, and sends it to our lungs for re-oxygenation.
Heart failure is a chronic and progressive illness in which our heart muscle cannot pump enough blood to the body’s other organs. The heart continues to work but not as efficiently as it should. As this happens, fluid backs up into the lungs and other body tissues and causes congestion and impaired function of major organ systems.
This subject will discuss how to describe heart failure and how it affects the heart and lungs. In addition, we will learn about the different types of heart failure, symptoms of heart failure, complications that may arise from it, and treatment options.
Epidemiology:
The current prevalence of chronic heart failure in the general adult population is 2–3%, with a higher prevalence in older age groups. In addition, chronic heart failure is responsible for 5% of emergency medical admissions and around 50% of admissions to hospitals for patients aged over 75 years.
Heart failure is common, and its frequency increases with age. Symptoms of chronic heart failure include breathlessness, ankle swelling and fatigue. The heart cannot pump sufficient blood due to coronary heart disease, hypertension, valvular dysfunction, or cardiomyopathy.
Many patients have a reduced ejection fraction on echocardiography. The primary management goals are to reduce symptoms, prevent progression and reduce further cardiac events (cardiovascular death, myocardial infarction, additional hospitalizations for heart failure).
Normal Functioning of Heart:
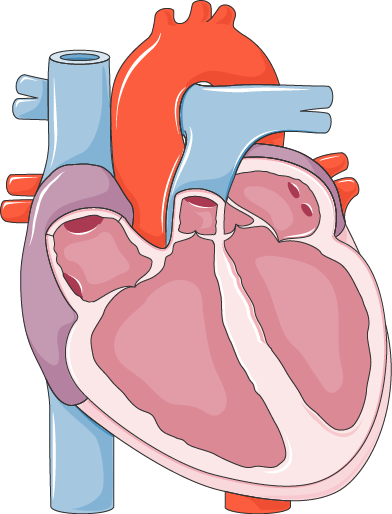
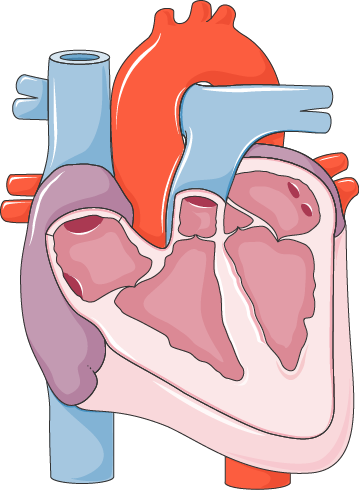
Our heart is a muscular pump made up of four chambers. The right side of your heart receives deoxygenated blood from your body and pumps it to your lungs, where it is oxygenated.
The left side of the heart gathers re-oxygenated blood from the lungs and pumps it to the body, and then the blood enters the right side of the heart, continuing the cycle.
The amount of blood pumped into the body depends on the demand of the blood by the body to sustain the required activity. The demand can be increased in case of increased physical work or decreased in resting conditions.
In good health, resting cardiac output is around 5 L/min, with a typical heart rate of 70 beats/min and stroke volume of 70 mL. Because the entire ventricle has an average capacity of 130 mL, the proportion expelled is more significant than half of the ventricular contents, with the leftover (residual) amount being around 60 mL.
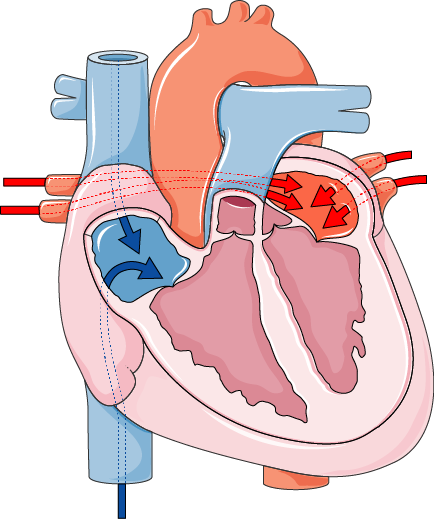
The right side of the heart receives blood from the body (Blue colour) & Left side of the heart receives blood from the lungs (Red colour)
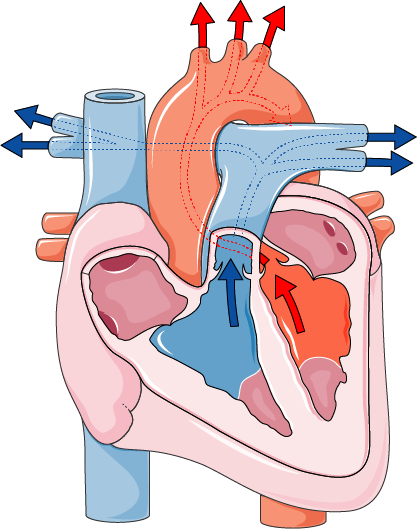
The right side of the heart pumps blood to the Lungs (Blue colour) & Left side of the pumps blood to the body (Red colour)
Cardiac Output:
Cardiac output, measured in litres per minute (L/min), is the volume of blood pumped from the heart at a particular time. Cardiac output depends on heart rate (HR) and stroke volume (SV).
An increase of any one of these factors can increase cardiac output. Product of heart rate and stroke volume combines to form cardiac output. It can be presented as:
CO = SV x HR
Our body’s autonomic nervous system controls the heart rate (HR).
Stroke volume (SV) is the blood ejected during the systole phase and depends upon the heart’s preload, afterload, and contractility. As the Frank-Starling mechanism, the ability of the heart to alter the force of contraction depends upon the preload.
Phases of Heart Contraction:
The heart is a two-beat pump consisting of two phases, the systolic and diastolic phases. The systolic phase is the first half of the heartbeat. The other half of the heartbeat is called diastole, or relaxation phase.
Systolic Phase:
The systolic phase is the heart’s contractile phase. Pressure and volume of the heart’s ventricles increase to pump blood out into the lungs for oxygenation and into the body for circulation. The heart’s systolic, or contraction phase, is when the heart squeezes blood into circulation.
As the heart contracts and empties, blood enters the arteries, causing pressure to rise inside them. The systolic pressure occurs during this phase and increases as the ventricles contract.
Diastolic Phase:
In the diastolic phase, the heart is not squeezing or pumping. Instead, it is relaxing and filling with blood so that it can pump again.
The relaxation phase occurs after the heartbeat. The heart’s left and right ventricles are fully stretched and ready to begin filling for the following contraction.
Blood flows into both chambers through their valves. In this phase, the heart is filled with blood, which has already been pumped through the lungs and deoxygenated blood from all over the body.
Types of Heart failure:
Heart failure is a clinical syndrome caused by any structural or functional impairment of ventricular filling (diastolic heart failure) or myocardial contraction (systolic heart failure).
It is characterized by an inability of the heart to supply sufficient blood flow to meet the metabolic needs of the body. There are two different forms of heart failure: systolic and diastolic. Based on whether left ventricular ejection fraction or filling pressures are most abnormal.
Systolic heart failure is characterized by reduced cardiac output and increased central venous pressure that may result from myocardial infarction, hypertension, or valvular disease.
In contrast, diastolic heart failure results from stiffened myocardium and impaired relaxation in the presence of normal systolic function. It most commonly occurs with hypertension but may also be associated with diabetes mellitus, hyperthyroidism, and other causes.
Left-sided heart failure results from impaired emptying of the left ventricle with elevated left ventricular end-diastolic pressure and elevated pulmonary pressure, causing dyspnoea on exertion.
Right-sided heart failure results from systemic venous congestion with ascites and oedema.
Systolic Heart Failure:
Systolic heart failure is when the heart muscles get weak and cannot pump blood efficiently from the ventricle to the body.
The word “systole” has been derived from the Greek word ‘systole’, where ‘systole’ means contraction.
The weakness in the heart muscles can be due to the death of cardiomyocytes (heart muscles); due to the end of cardiomyocytes, the ventricle size increases and the muscle mass of ventricles decreases.
Thinning of ventricle walls occurs, due to which enough force is not generated to empty the ventricle.
Increased ventricle size and thinning of ventricle walls
Ejection Fraction:
Ejection fraction is a standard measurement of heart failure.
“It measures the percentage of blood pumped out of your left ventricle with each heartbeat.”
When an ejection fraction is 55 per cent or greater, it is considered normal, whereas 25-55 per cent is considered low or impaired ejection fraction. (IEF). IEF indicates that your heart weakens over time, leading to heart failure.
Ejection fraction can be calculated as:
Volume of Blood Ejected / Total Volume of Blood in Ventricle x 100 = EF
Measuring ejection fraction using echocardiography is the most effective and frequently used test for detecting systolic heart failure.
Ejection Fraction is a clinical parameter used to measure the contraction of the left ventricle. This can be useful in identifying and staging heart failure and monitoring its treatment.
Causes of Systolic Heart Failure:
The underlying diseases causing systolic heart failure are:
- Heart Muscle disease (cardiomyopathy)
- Coronary Artery Disease
- Valvular Disease
- Regurgitation
- Stenosis
- Arrhythmias
Systolic heart failure may lead to shortness of breath, tiredness, swelling of the legs etc. To avoid systolic heart failure, factors like smoking, obesity, hypertension and improper diet must be avoided with proper exercise and proper medication.
Diastolic Heart Failure:
Diastolic heart failure occurs when our heart is unable to fill with enough blood during diastole or the rest of the heart.
The ventricles of the heart do not fill with a sufficient blood volume during diastole. Hence, there is a reduction in the volume of blood pumped out from the heart in systole.
Diastolic Heart Failure is caused by the thickening of heart muscles, which reduces the space in the cardiac ventricles and causes less blood to be pumped into and out of your heart with each beat, resulting in less blood flowing to your body.
Hypertrophy of Ventricle walls and reduced ventricular filling space
In diastolic heart failure, the ejection fraction is preserved, but it’s overall reduced. Diastolic heart failure is also known as HFpEF for heart failure with preserved ejection fraction.
It is more common among older adults with high blood pressure. The thickening of muscle tissue in the left ventricle can be caused by long-term pressure in the arteries (chronic hypertension) or previous heart attacks.
Heart failure does not indicate that your heart has stopped functioning. It means the heart does not pump as vigorously as it should. As a result, the heart stiffens and cannot relax and fill properly.
People with diastolic failure may develop symptoms slowly or even have no symptoms. Diastolic failure can be challenging to diagnose because it develops gradually and has few signs in the early stages.
Diastolic heart failure is a secondary disease caused as a result of already present chronic diseases like,
- Chronic Hypertension
- Aortic Stenosis
- Cardiomyopathy
Left-Sided Heart Failure:
The left side of the heart gathers re-oxygenated blood from the lungs and circulates it throughout the body. Left heart failure occurs when your heart’s left side is too weak to pump out all the blood that returns to it.
If left-sided heart failure is not treated, it can cause right-sided heart failure, which can, in turn, lead to death.
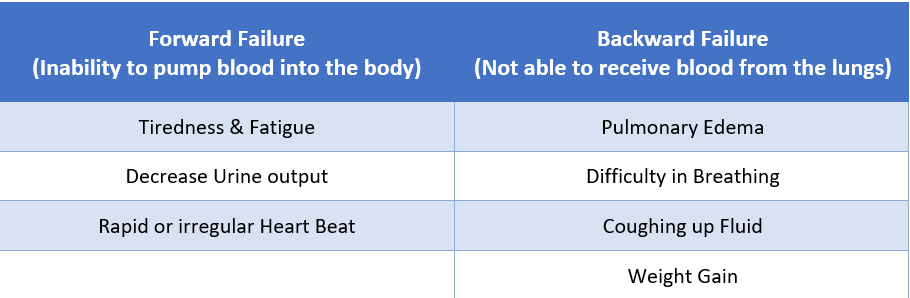
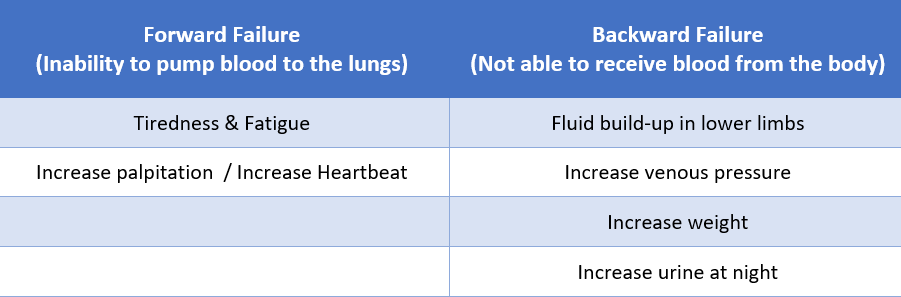
Symptoms of Left-Sided Heart Failure:
Right-Sided Heart Failure:
Right-Sided Heart Failure is a condition
where the right ventricle fails to pump enough blood to meet our body’s
requirements.
Right-sided heart failure refers to
congestive heart failure where the right ventricle of the heart fails to supply
enough blood to meet our body’s requirements. Although fluid can accumulate in
any part of the body, it tends to gather in the lower limbs due to gravity when
standing up. This causes oedema (swelling) in both legs and feet and congestion
in the liver, resulting in a swollen abdomen.
Symptoms of Right-Sided Heart Failure:
Compensation and Decompensation Phenomenon in Heart Failure:
Heart failure is a chronic and progressive illness in which the heart muscle cannot pump blood to meet the body’s needs. The heart is a very clever organ; while it becomes less efficient, the body has mechanisms that can compensate for some time to maintain sufficient blood flow.
Eventually, these compensatory mechanisms fail and lead to worsening symptoms.
One of these compensatory mechanisms is the ability of the heart to increase its overall pumping ability (cardiac output) through a combination of increasing overall heart rate (the number of beats per minute) and increasing stroke volume (the amount of blood pumped out with each beat).
Following are the compensatory mechanism which is activated as the result of heart failure:
Activation of Sympathetic Nervous System:
Sympathetic nerves release neurotransmitters of the heart, which can excite and reduce the strength of the heart. In heart failure, the sympathetic nervous system acts by causing an increase in heart rate and contractility of the heart by the release of neurotransmitters.
This increase in cardiac output delivers a sufficient amount of blood to various tissues, which need a continuous supply of oxygen and nutrients.
Increase Preload:
Frank’s starling equation states that cardiac output is directly related to preload and stroke volume.
The heart is a pump that can increase stroke volume to meet the increased metabolic needs of the body. Preload increases the ability of heart muscle to employ more passive stretch in ventricles. So increased preload or pre-stretch of myocardial cells will help develop greater force in the following systole.
ADH promotes water reabsorption from distal tubules and collecting ducts causing the urine to become more concentrated. The blood volume increases, which causes the left ventricle to fill more completely in diastole, increasing the preload without affecting stroke volume.
Myocardial Hypertrophy:
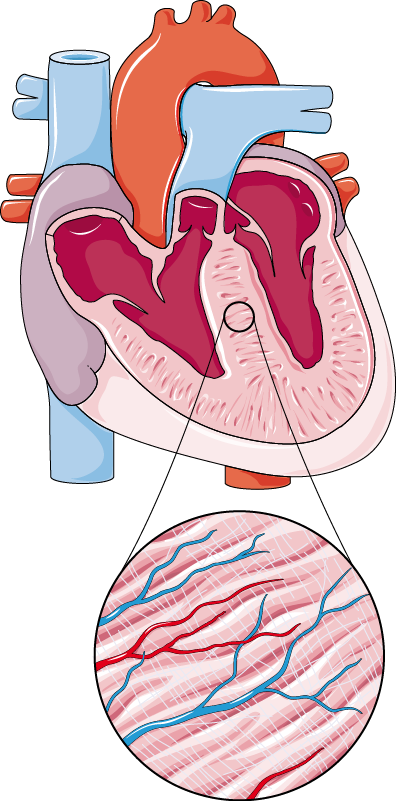
Myocardial hypertrophy refers to the thickening of the heart muscle and results in an increase in heart muscle mass in response to the elevated workload on the heart. This cardiac enlargement is a compensatory mechanism to keep up with the body’s increased demand for oxygen due to high blood pressure. Myocardial hypertrophy most commonly affects the left ventricle, the chamber of the heart that pumps blood to all regions of the body.
Decompensation:
But heart cells are not getting enough oxygen in heart failure, so the cells start to die off, and this compensation mechanism also fails.
Also, due to myocardial hypertrophy, ventricular space decreases, which reduces blood filling space in ventricles.
All of the above compensatory effects result in a short-term increase in cardiac output but progressively fails to meet overall demand.