What is Insulin?
Insulin is a hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food you eat for energy or store glucose for future use. Insulin helps keep your blood sugar level from getting too high (hyperglycemia) or too low (hypoglycemia).
The cells in your body need sugar for energy. However, sugar cannot go into most of your cells directly. After you eat food and your blood sugar level rises, cells in your pancreas (known as beta cells) are signalled to release insulin into your bloodstream. Insulin then attaches to and signals cells to absorb sugar from the bloodstream. Insulin is often described as a key because it unlocks the cell to allow sugar to enter and be used for energy.
How is insulin secreted from Pancreas?
Insulin is an endogenous hormone released from the beta cells of our pancreas in response to various stimuli, especially while eating food consisting of carbohydrates or sugary substances. Insulin is also released from hormonal stimulation like GLP-1, glucagon, cholecystokinin, high concentrations of fatty acids.
Some drugs are also responsible for the increase in insulin release, like sulfonylurea, meglitinides etc.
Mechanism of Insulin Release
Insulin is released from pancreatic beta cells. In hyperglycemic conditions, there is an increase in intracellular ATP levels inside pancreatic beta cells. This increased ATP levels close the potassium channel inside the cell, which stops the movement of potassium outside the pancreatic beta-cell resulting in depolarization of the cell.
The depolarization of the cell opens the calcium channel and causes the inward movement of calcium through its medium. The inward movement of calcium results in increased intracellular calcium levels, which trigger insulin secretion outside the beta cells.
Once insulin is released from the pancreatic beta cells, it enters the blood circulation. It interacts with its target cells, usually the liver, muscles, and fatty tissues, and produces its effect. The net result of insulin is made when it attaches with its receptor on the target cells.
Insulin causes the glucose channel to open on the cell’s surface upon interacting with its receptors. The glucose can be transported inside the cell with the help of glucose transporters.
Once glucose is transported inside the cell, it is stored as an energy source and used in different metabolic functions of tissues, cell growth, cell division, DNA synthesis etc.
Types of Insulin:
There are many types of insulin preparations available for diabetic patients. They differ based on their onset of action, peak effect and duration of action. Based on these factors, insulin can be divided into the following categories:
Fast-acting insulin:
As the name indicates, insulin preparations show their effects faster than other insulin preparations. Fast-acting insulin can be divided into different two types.
Regular insulin:
It is synthesized in the laboratory and equivalent to endogenous insulin. This short-acting insulin shows effects 30 minutes after subcutaneous injection. The Peak effect can be seen in two to three hours, and the effective duration is up to 6 hours.
Regular insulin is in crystalline form, and due to this Crystalline form, it takes time to show is its effect hence it is given 30 minutes before a meal. Examples are,
Insulin R (Human Insulin)

Regular insulin is usually administered intravenously in the treatment of diabetic ketoacidosis and also before operations of diabetic patients to control their high blood glucose levels.
Rapidly acting insulin:
These insulin analogues show their effect within 10 minutes of their subcutaneous injection. Their peak effect can be seen in two hours, and in four to 8 hours, their effect diminishes.
Rapid-acting insulins are soluble insulins immediately absorbed and taken up by the bloodstream. As absorption of rapid-acting insulin is fast and readily soluble, they are injected directly before a meal.
- Insulin Lispro (Brand – Humalog)
- Insulin Aspart (Brand – Novolog Felxpen)
- Insulin Glulisine (Brand – Apidra Solostar)
These are examples of rapid-acting insulin.
Intermediate-acting insulin:
Intermediate-acting insulin in which human insulin is combined with either protamine or zinc, forming a complex that dissociates over time after subcutaneous injection.

These are in biphasic solution and do not mix, having a cloudy appearance. After injection, they show extended activity, and their usual onset of action is 1-2 hours, and peak effect can be seen from 4 to 8 hours. They are administered twice a day. Example
Insulin NPH – (Human insulin with Neutral Protamine Hagedorn)
Long-acting insulin:
These long-acting insulin analogues show their effect over an extended 24 hours. They have been developed using DNA recombinant technology. They do not show peaks in their effect as seen in other types of insulin.
Following are long-acting insulin:
Insulin Glargine:

Insulin glargine is formulated at a slightly acidic pH of 4. Upon injection, the insulin glargine forms a micro precipitate in the neutral pH of the body. This precipitation causes the slow release of insulin from the injection site into the bloodstream.
Insulin glargine has onset from three to five hours, and its duration of action is 24 hours. Insulin glargine doesn’t show a peak effect and has a sustained action duration with more predictable flat profiles.
Insulin Detemir:

Insulin detemir is formulated at neutral pH. Once injected subcutaneously, it is absorbed and reversibly binds with human albumin becomes inactive. It is then released slowly from the albumin to produce its effect. The longer duration of action is due to the dissociation of insulin from albumin.
Like insulin glargine, it also shows onset from three to five hours and 24 hours of action without showing peak effect and having a predictable flat profile.
Insulin Degludec:

Insulin Degludec forms a soluble depot upon the injection site, slowly and evenly absorbed by the bloodstream. Its duration of action is beyond 42 hours and due to sustained duration of action ends flexibility in dosing times. It is beneficial and shift workers and those patients who don’t have access to their insulin frequently.
How is insulin administered?
Insulin is available in only injectable form because it cannot be taken in pill capsules or liquid. After all, oral administration of insulin causes the breakdown of insulin in the stomach environment.
Muscular insulin injection is too painful and does not reduce overall blood glucose. Intravenous insulin delivery is only used in emergency cases like diabetic ketoacidosis or a hyperosmolar state.
Intravenous insulin administration is not routinely recommended for those patients who can eat and drink.
Site of Insulin Injections:
Insulin needs to be injected under the skin, also called subcutaneous injection, to show its effect. Any area of the body with loose skin is utilized. As long as skin is clean, wiping it with alcohol is not necessary.
Absorption of insulin varies from site to site of a distraction. The absorption of insulin from the abdomen is the fastest than from the arms, buttocks absorption is on second last, and the absorption from thighs is the slowest.
The insulin injection site is changed every time to avoid tissue injury or damage to the skin.
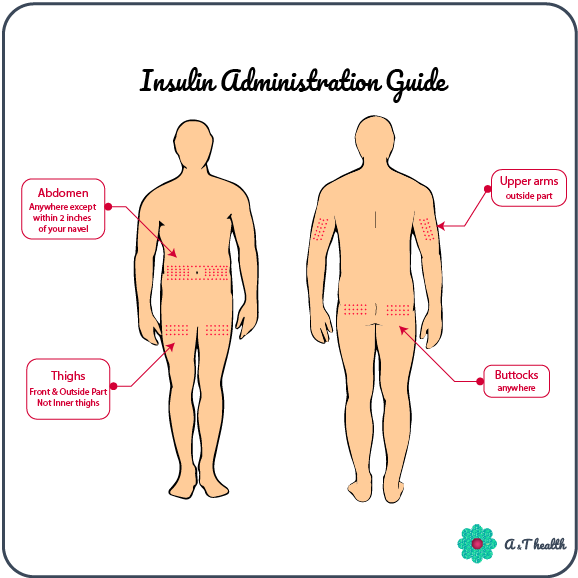
Following are the common sites of injection used for injecting insulin;
- Outside part of the upper arms
- Buttocks
- Front and outside part of the thighs (do not inject insulin in inner thighs or right above the knee as it is painful and there is usually not enough fat on these areas, but some people who have fat in this area can inject)
Insulin Pumps:
Insulin pumps are used in those diabetic patients who require multiple injections of insulin in a day. Insulin pumps are devices that can be worn outside with the connecting tube inserted in the body with the help of a needle. At different times of the day, the pump can be configured to deliver a varied infusion rate according to the patient’s needs configured in the pump settings.
Choosing insulin Syringes and Needles:
- Plastic disposable syringes come in 0.3ml, 0.5ml and 1ml sizes. Choice of syringe depends upon the quantity of insulin to be administered and varies from patient to patient. 0.3ml and 0.5 ml mainly are used.
- The needle length varies between 6mm, 8mm, and 12.7mm. Long size needles are used in patients who are obese so that there is no variation in absorption of insulin.
- Needle thickness varies from 28, 30, 31 gauges, 28 is the thickest and 31 is the thinnest and almost painless.
- Syringes are to be used by one individual only.
- For one individual syringe can be reused until blunting of the needle occurs.
- Recap the needle after each use to avoid contamination.
Insulin Safety:
- Extreme temperatures degrade the structure of insulin, turning it useless. So, insulin should be stored in a cool and shady place.
- Never keep insulin in direct sunlight in areas with high temperatures like in a car dashboard or kitchen.
- Never freeze the insulin or place it in the refrigerator for storage. Freezing the insulin also makes it useless.
- Insulin can be safely stored at room temperature for up to 28days after opening. Before opening, keep insulin in the refrigerator.
- Insulin vials can be kept in the refrigerator if insulin lasts longer than 30days.
- For the exact storage conditions, always follow the manufacturer guidelines as they are specific for each type.